Audit and inspections are critical methods in achieving compliance. Both are systematic, and documented processes conducted to verify that a certain set of standards, guidelines and procedures are being met; however, they are used interchangeably according to their processes.
As an FDA Investigator, the term “inspection” was used most often; however, as I ventured out into the industry to work for sponsor companies and CROs, I heard both terms “audit” and “inspection” used interchangeably depending on who was conducting them. At the same time, professional organizations like ASQ (American Society for Quality) primarily used the term “audit”.
According to the sponsor companies I have worked for in the industry, the term “audit” is used when it is conducted either internally within the organization or externally with a supplier. The term “inspection” is used when conducted by a regulatory authority such as FDA, EMA, ISO, etc.
So, what’s the difference?
Inspection vs Audit
Regulatory Authorities such as the USFDA(United States Food & Drug Administration), EMA (European Medicines Agency), etc. use the term “inspection” which is routinely done to:
- Determine the safety and protection of subjects
- Ensure adherence to federal regulations
- Determine the validity of clinicals trials supporting approval applications
According to professional organizations like ASQ (American Society for Quality), everything is considered an audit broken down into different types (e.g., process, product, system, etc.) and parties such as:
- First-party audit
- Second-party audit or
- Third party audit
First party audits, or internal audits, are conducted within an organization to measure its strengths and weaknesses against its own procedures and processes against external standards.
Second party audits, or supplier audits, are conducted externally on a supplier by a customer to determine that products are being handled properly according to the customers’ procedures / industry stands and services are done according to the requirements of contractual agreement.
Third party audits are conducted independently from outside organizations or regulatory authorities and can result in certification, registration, recognition, approval, etc.
According to the sponsor companies I have worked for in the industry, the term “audit” is used when it is conducted either internally within the organization or externally with a supplier. The term “inspection” is used when conducted by a regulatory authority such as FDA, EMA, ISO, etc.
Key Takeaway
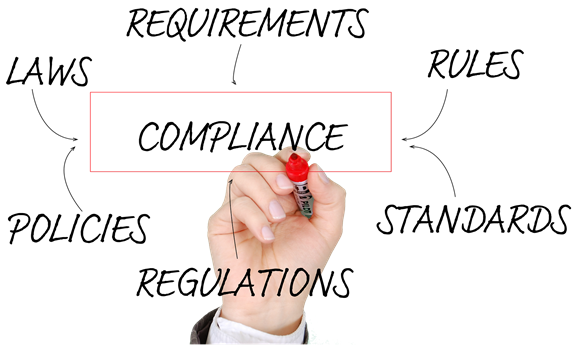
The best way to minimize confusion is to consider First and Second party audits conducted internally or externally by clients or consultant companies as AUDITS and Third-party conducted by regulatory authorities as INSPECTIONS both with the ultimate goal to achieve compliance and adherence to set standards, guidelines and procedures.
How are audits and inspections differentiated in your company or department? Feel free to contact us with your comments, questions or feedback. Looking forward to hearing your thoughts on this topic!